Being aware of risk factors, and especially of your own risk factors is really important in helping you to avoid and protect yourself from thrombosis.
A venous thromboembolism (VTE), often referred to as a deep vein thrombosis (DVT), pulmonary embolism (PE), thrombosis or blood clot, is a clot that forms in a vein.
Around 50%-60% of blood clots are associated with being admitted into hospital. This can be due to becoming immobile for a period of time, treatments you received or undergoing procedures during your stay.
All hospitals are expected to complete a DVT risk assessment for every patient admitted into hospital – whether as a planned admission or following an urgent or acute admission. Risk assessing an individual is very simple and involves a healthcare professional reviewing a series of questions that help lo assess a patient’s risk level and if any therapies or actions need to be taken to reduce their risk.
If you are admitted into hospital, you should be Risk Assessed for Blood Clots
Your risk of developing a blood clot may increase if you are admitted into hospital as an emergency admission, a planned admission for a procedure, or if you are receiving treatment. It is helpful to talk with your health care professional about your VTE risk and what can be done to reduce.
Things to reduce the risk may include:

Having cancer and receiving certain treatments for cancer, might mean that you have a higher risk of developing a blood clot. This could be due to a number of things.
The type of cancer:
Cancer cells produce and release substances that stimulate the blood to make more clotting factors.
There are several known cancer types which increase the risk of developing a blood clot such as cancer of the:
Cancer treatments:
Certain treatments can increase the risk of developing blood clots.
When chemotherapy kills cancer cells the cells can also release substances that cause more blood clotting
The hormone drug tamoxifen is also known to increase the risk of blood clots.
The newer immunotherapy treatment may also increase the risk of blood clots.
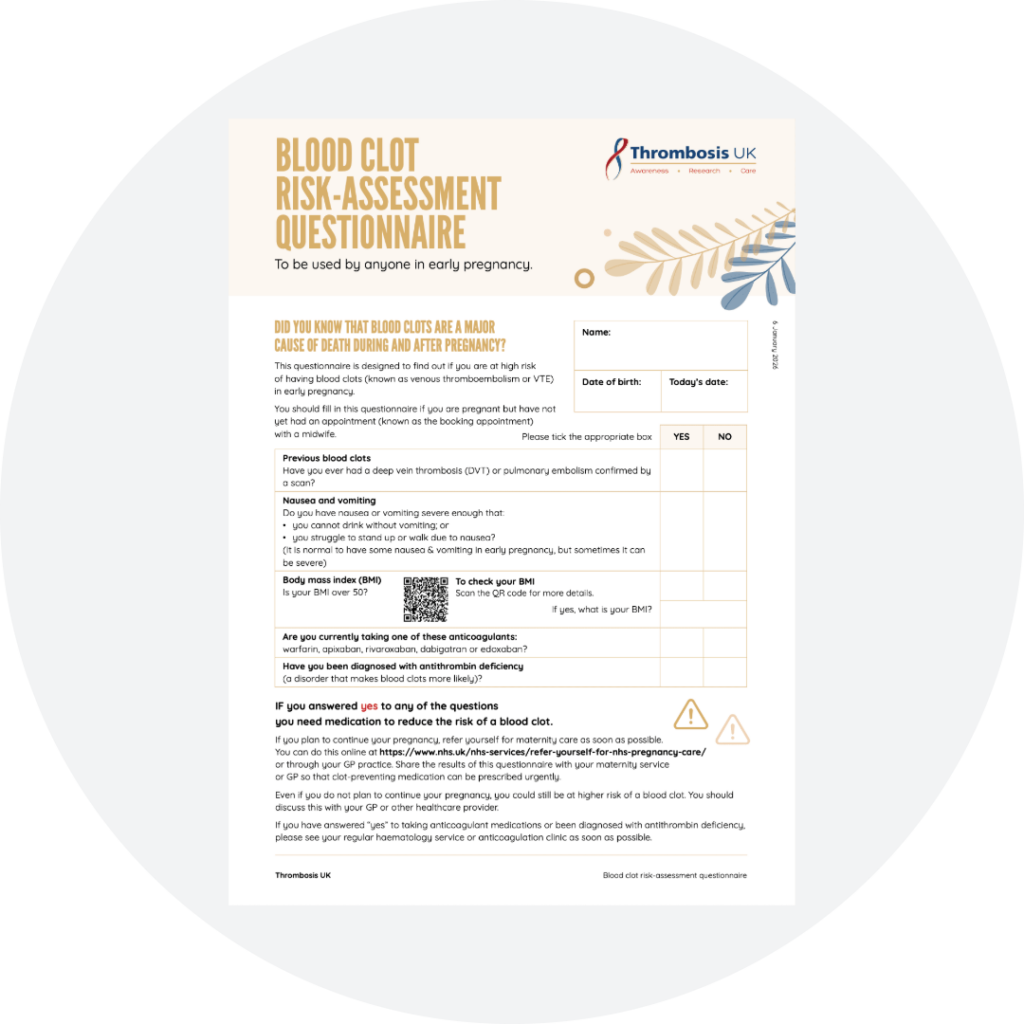
Thrombosis UK is partnering with NHS England to improve the prevention of blood clots in early pregnancy. This questionnaire is designed to find out if you are at high risk of having blood clots (known as venous thromboembolism or VTE) in early pregnancy.

Pregnancy can increase the risk of venous thromboembolism (VTE) 4- to 5-fold over that in healthy but non pregnant females.
During pregnancy, blood clots more easily. This is partly to keep you safe because it reduces the risk of excessive blood loss when giving birth.
A pregnant person may also experience less blood flow to the legs later in pregnancy because the blood vessels are compressed by the growing baby, and this can increase their risk.
Although anyone can develop a blood clot, a pregnant person is at higher risk for developing a blood clot during pregnancy, childbirth, and up to 3-months after delivering a baby.
Hormone therapies can bring many benefits, however, some types of hormones and the way they may need to be taken can increase the risk of developing a blood clot.
The most common areas where hormone therapy and increased risk of blood clots will need to be considered are:
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]
Applications are accepted on the basis that Thrombosis UK can share the content with external judges who will assist us with assessments. Service models, resources and working processes of successful Thrombosis UK VTE Award winners will be uploaded to the Thrombosis UK website and shared via publications, social media, and other opportunities.
When completing your application form, you should use lay language and answer each question in a concise manner.
Please keep to any word limits given.
All sections need to be completed, if any section is removed, omitted or incomplete, we cannot process the application.
Applications need to be submitted via email to: [email protected] You will receive a notification of receipt within 48 hours of submission. If you do not receive a notification, please email [email protected]
The closing date for applications is 1st February 2025
We are unable to consider late applications.
Thrombosis UK has a strict data protection policy that complies with UK data protection law.
Your name and contact details may be stored for up to 12 months in order for correspondence relating to your application be appropriately processed.
We wish to make you aware that your name and contact details, as included on your completed application form, will be viewed by the Thrombosis UK appointed Judging Panel solely for the purpose of reviewing and assessing your completed application. If your nomination is short listed, a representative from Thrombosis UK will then seek your permission to include your name on the summary paragraph included in the awards brochure and on the Thrombosis UK website.
Thrombosis UK takes security and confidentiality very seriously. Your name and contact details will never be passed or shared with any third party or an unauthorised individual. If you have any queries, please contact: [email protected]